Understanding the Process of Bone Marrow Transplantation
Particularly in the field of oncology, bone marrow transplantation is a highly effective treatment, more notably in the cases of bone cancer and bone marrow cancer. The difficult process involves the transplantation of healthy stem cells that can take the place of damaged or diseased bone marrow. This article talks about the intricate details of bone marrow transplantation and why it is so important in treating bone marrow cancer.
What is a Bone Marrow?
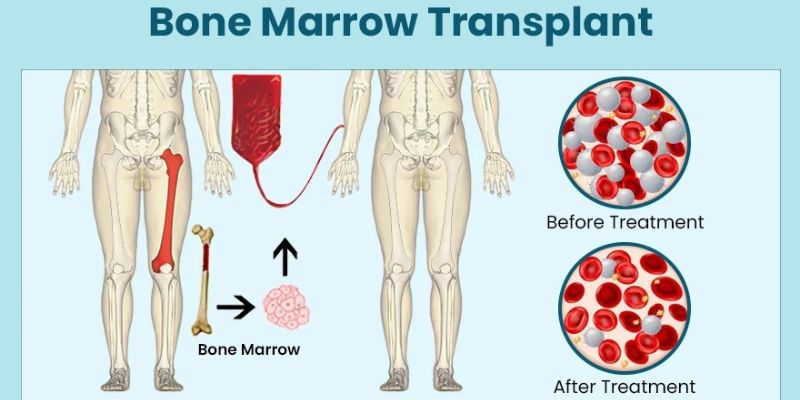
Bone marrow, the soft, spongy tissue situated inside bones, is a pivotal product of the human body's hematopoietic system. It is the one that produces the cells of blood, such as red blood cells (erythrocytes), white blood cells (leukocytes), and platelets. The red and white blood cells have three major functions:
1. Oxygen delivery
2. The immune response,
3. Clotting.
What do you mean by Bone Marrow Cancer?
The bone cancer concept refers to cancers that originate from bone tissue. These can be either primary, of bone origin, or secondary, that is, originating in other body regions. Interestingly, multiple myeloma, which is also called bone marrow cancer, involves abnormal cell divisions in the bone marrow.
Why Do You Need a Bone Marrow Transplantation?
Bone marrow cancer treatment is required for several reasons, mainly related to the removal or improper functioning of the bone marrow. Here are some typical indications for bone marrow transplantation:
1. Hematologic Cancers: This treatment model is commonly used in haematological malignancies like leukaemia, lymphoma and multiple myeloma. They may suppress normal blood cell formation in the marrow, decreasing the number of healthy red blood cells and thus weakening the immune system. Transplantation intends to substitute the unwanted marrow with healthy donor cells capable of replacing the damaged ones with cancerous cells and to restore normal hematopoiesis.
2. Bone Marrow Failure Syndromes: Bone marrow failure is a rare condition caused by cancer or noncancerous disorders that disrupt the normal function of the marrow and impair its ability to generate enough blood cells. Such treatment has a potential cure since faulty marrow is replaced with physiological marrow that produces normal blood cells.
3. Genetic Disorders: Some inherited genetic diseases disrupt the natural functioning of the marrow. Other conditions include sickle cell disease, thalassemia, and severe combined immunodeficiency (SCID). In such situations, bone marrow cancer treatment offers a chance to handle the condition by infusing the healthy donor cells with corresponding normal genetic encoding, which is able to correct bone marrow dysfunction.
4. Immune System Disorders: Patients with some immune system disorders may have defective immune organs like the bone marrow, which is unable to produce immune system cells normally. Bone marrow transplantation can, in turn, restore normal immune system functions by introducing healthy donor cells bearing the ability to generate immune cells functioning at a high level.
5. Chemotherapy or Radiation Therapy: In some cases, high-dose chemotherapy or radiation therapy may injure bone marrow and cause poor blood cell production resulting from the absence of healthy blood cells. It is one of the treatments of choice to rescue the damaged bone marrow and restore normal function following intensive therapies.
Types of Bone Marrow Transplantation
Autologous Transplantation: In this approach, the patient's cells (either bone marrow or stem cells) are harvested, preserved, and then reintroduced to the patient after receiving intensive chemotherapy or radiation therapy. The therapy's purpose is to destroy cancer cells and rebuild the retained bone marrow function.
Allogeneic Transplantation: Allogeneic transplantations entail a transfusion of healthy bone marrow or stem cells obtained from another genetically related donor, usually the patient’s brother or a random donor. This protocol provides such benefits, namely, immune system rejuvenation and the likelihood of graft-versus-tumour effects when the donor immune cells conquer the residual cancer cells.
The Process of Bone Marrow Transplantation
Preparation: Before transplantation, the patients are subjected to a complex medical evaluation to discover the details of their overall health status and correlate this with their suitability for transplantation. This investigation includes tests to determine the nature of the organ function, the extent of the disease, and the compatibility between the donor and recipient.
Conditioning Regimen: Patients receive the highest dose of chemotherapy and/or total body radiation to kill all the cancer cells and leave much room for donor cells to repair and thrive in the bone marrow after replacing germinal cells. Immunosuppressive drugs in the preparation protocol also suppress the recipient's immune system to prevent the donor cells from being rejected.
Transplantation: After transplant training, the next step is for the patient to receive the donor's bone marrow or cells via intravenous infusion. The transfused cells move to the bone marrow area and expand afterwards, with a repeat tumour hematopoietic system.
Engraftment: Transplantation, i.e., engraftment, is the attainment of donor marrow cells in the patient’s bone marrow, thereby improving the number of healthy blood cells in their bloodstream. Evaluation of engraftment encompasses frequent blood sample analysis that concerns donor cell presence detection and recovery of blood counting.
Recovery and Follow-Up: During and following a transplant, patients are monitored for GVHD (graft-versus-host disease), infections, and organ toxicities that could cause severe complications. Evaluation-wise, the long-term follow-up stresses the effectiveness of the treatment, cancels the repercussions of side effects, and helps the patients adapt to the recovery process.
Challenges and Complications
Bone marrow cancer treatment also brings along with some additional complications and challenges. On that note, the possibilities of graft failure, graft-versus-host disease (GVHD), infections, organ toxicity, and disease progression or relapse should be considered. The complexities of managing these disorders necessitate the involvement of a multidisciplinary approach, including specialists from oncology, haematology, transplant specialists, infectious diseases and supportive care teams.
To Sum Up
Bone marrow transplantation, despite all its complexity, is one of the most important methods of treating bone cancer, bone marrow cancer, and any blood disorders. By activating the curative capabilities of disease-free donor cells, the treatment promises to achieve a probable remission of the disease and long-term survival. Nevertheless, it is based on selective and detailed patient screening, excellent care and continuous research to repeat and improve results and, hence, minimise complications.






